The number of people with Acquired Brain Injury is increasing, but the support for them is not keeping up with demand. There were over 356,600 admissions to hospital with brain injury in the UK in 2019–20, an increase of 12% since 2005–6 (1). While many people will be discharged without needing further treatment, research shows that 50% of people with a traumatic brain injury will experience further decline in their daily lives (2). Acquired Brain Injury (ABI) has been described as a ‘hidden epidemic’ affecting many thousands of people, yet the number of available neurorehabilitation beds across the UK is ‘inadequate’ (3).
There were over 356,600 admissions to hospital with brain injury in the UK in 2019-20, an increase of 12% since 2005-6.
Experiencing a head injury is much more common than people realise. The main causes are falls, an external blow to the head, road traffic accidents and assault. There are more men than women with an ABI and veterans are among the groups who are more likely to suffer with this lifelong condition. It is increasingly well known that repeated concussion, similar to that which can be sustained playing sport, can lead to progressive degeneration known as Clinical Traumatic Encephalopathy (CTP), which puts people at increased risk of dementia. In fact, there is a known association between ABI and dementia, with the younger the age when the brain injury occurred, the greater the likelihood of dementia in later life.

Depending on the severity of the injury, the post trauma effects of ABI present many challenges for the individual, their family and the services that support them. They may experience long lasting effects such as depression, aggression, epilepsy, weight gain, loss of cognitive function – conditions that require specialist intervention and, in some cases, long term care. The effects are often not obvious and ABI has been described as an ‘Invisible Syndrome’. People living with ABI can suffer from social isolation, relationship breakdown and frustration as they try to get people in their everyday life, and even clinicians, to take their predicament seriously (4).
It goes without saying that prevention is one of the most effective ways of reducing the impact of ABI on the population and this is a public health issue. However, the 1.3 million people in the UK living with a brain injury need support from specialists.
1.3 million people in the UK are living with an Acquired Brain Injury
Early access to neurorehabilitation is a very effective way of helping patients to regain functioning and even exercise and other lifestyle changes have been shown to result in improvement, due to their anti-inflammatory effects.

Neurorehabilitation should be implemented after an individual’s immediate medical needs have been met. It supports the safe transition of the individual back to the community, thus relieving pressure on acute beds, and helps the person to maximise their potential. There is considerable regional variation in access to specialist rehabilitation and often people suffering from ABI are not cared for in an environment that specialises in their condition. Acquired Brain Injury falls outside of the Care Quality Commission (CQC) list of service user bands, although CQC will expect the operator to have the specific knowledge, skills, training and facilities to support any service users with ABI, and for the operator to include such in their Statement of Purpose if they are doing so (5).
Carterwood’s own database shows there are approximately 200 organisations in the independent sector, providing just over 5,000 specialist beds, for people living with neuro-disability such as ABI, with considerable regional variation. There is a well-documented shortfall in support for individuals and their families and a real opportunity for operators to increase the provision of neurorehabilitation, respite and long-term care for this group. The All-Party Parliamentary Group on ABI calculates that 14,600 neurorehabilitation in-patient beds are needed for the annual caseload of 300,000 ABI admissions [Carterwood note: this exceeded 350,000 for 2019-20]. Currently there are only 4,600 beds available in the UK and, while the independent sector has increased its bed capacity by 700, the NHS has lost 100 beds since 2013 (6).
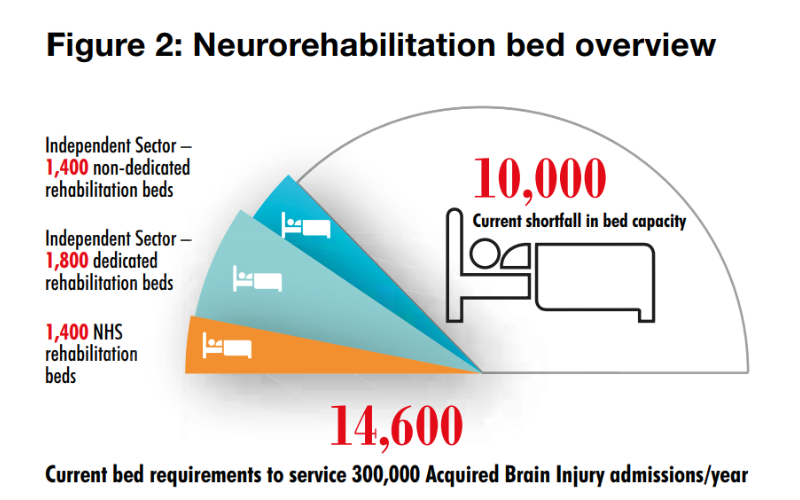
Image: Time for Change APPG on ABI 2018
When developing specialist services, a number of considerations are needed. All care providers need to be able to recruit, train and retain sufficient (health and care) staff, which makes location crucial. Specialist ABI services will additionally need to recruit and deploy a multi-disciplinary team comprising of psychologists, physiotherapists, occupational therapists, speech and language therapists and social workers. Good relationships with primary care and local services are equally important.

A standardised assessment tool – such as the Mayo-Portland Adaptability Inventory-4 (MPAI-4) will be deployed. Perhaps most importantly, operators should not make the mistake of confusing a specialist service for people with a brain injury with services designed for people with a learning disability. Supporting people living with ABI in their recovery is as much about where the person came from, the person they were before, as it is about the functional impairment and predicted outcomes caused by the injury, and the support they require is very specialised.
The shortfall in specialist long term care and support for people living with ABI presents a real challenge for the UK and at the same time is an opportunity for operators to fill the gap and help to maximise the potential for people living with this condition. Carterwood have developed considerable expertise in supporting those operators, developers and investors in this specialist sector that wish to provide services that have the capability, are of the right size and in the right location to best deliver for this population.
If you want to expand your services or explore this opportunity, please get in touch with our sector-specialist experts.
Contact Form
Author: Alex Taylor, director at Carterwood

Sources
2 CDC (Centre for Disease Control) US
3 APPG (All-Party Parliamentary Group)
4 Journal of Long Term Care 2019
5 CQC 2023
6 Time for Change APPG on ABI 2018








